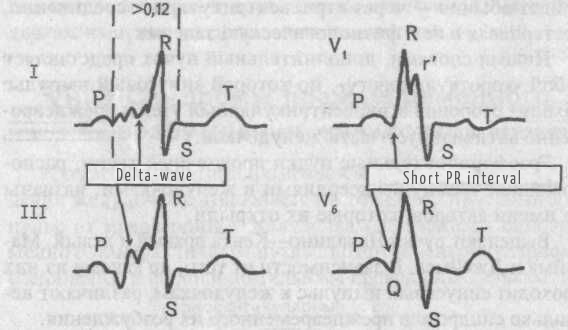
Short PR interval (Clerk-Levy-Cristesco syndrome (CLC syndrome))
Syndrome of the shortened P-Q (R) interval (CLC syndrome) occurs due to the presence of an accessory anomalous pathway of conduction of electrical impulse (the bundle of James) between the atria and the bundle of His. Sometimes this syndrome is called LGL syndrome (Launa-Ganong-Levin).
Causes: CLC syndrome is a congenital anomaly. Patients with this syndrome have an increased tendency to develop paroxysmal tachyarrhythmias.
ECG - signs:
- Shortening of the P-Q (R) interval, the duration of which does not exceed 0.11 sec.
- Absence of an additional excitation wave in the QRS complex (delta-wave).
- Presence of unaltered (narrow) and undeformed the QRS complex (with the exception of cases of the bundle branche block).
The development of CLC syndrome is accompanied by the appearance of sudden attacks of palpitations (paroxysms of supraventricular tachycardia). Paroxysmal arrhythmia in this type of ventricular pre-excitation occurs less frequently than in patients with the Wolff-Parkinson-White syndrome (WPW syndrome).
Paroxysmal supraventricular tachycardia is clinically manifested by a sudden onset of palpitations with a heart rate of 140 to 220 beats per minute (often 150 to 180 beats per minute). Before this, the patient sometimes feels a jolt in the region of the heart or neck. The palpitation may be accompanied by dizziness, noise in the head, compressing pain behind the sternum, fainting. In some cases, sweating, bloating, nausea, or even vomiting appears. At the beginning or at the end of a long paroxysm of arrhythmia, there may be profuse urination. The bout can be stopped with the help of vagal tests: exertion on the inspiration, lowering the face in cold water with a delay in breathing, massage the area of the carotid sinus on the neck. In rare cases, CLC syndrome may be accompanied by paroxysmal atrial fibrillation (frequent irregular heartbeats).